Module 5: Sleep Hygiene
Sleep is not a luxury; it’s the cornerstone of recovery, resilience, and optimal performance. For first responders in Alberta, however, quality sleep is often the first casualty of shift work, unpredictable calls, and the lingering effects of high-stress situations. This module provides critical strategies for optimizing your sleep, even with erratic schedules, helping you regain control over this vital aspect of “1st Health.”
Think of sleep as your body’s essential maintenance cycle. Without enough quality sleep, your physical and mental systems begin to break down, impacting your judgment, mood, and long-term health.
The Science of Sleep and the First Responder
Your body has a natural, internal clock, but your job often forces you to work against it. Understanding this conflict is the first step to mitigating its effects.
Circadian Rhythm Disruption: Fighting Your Internal Clock
-
- Your circadian rhythm is your body’s natural 24-hour sleep-wake cycle, primarily regulated by light exposure and hormones like melatonin. It tells you when to be awake and when to be asleep.
- The First Responder’s Challenge: Shift work (rotating shifts, 12-hour shifts, 24-hour shifts), night calls, and unexpected overtime fundamentally disrupt this natural rhythm. Your body is biologically programmed to be awake during the day and asleep at night. When you’re forced to work against this (e.g., sleeping during the day after a night shift), your body struggles to produce melatonin at the right time, leading to difficulty falling asleep and staying asleep.
- This constant disruption can lead to Shift Work Sleep Disorder (SWSD), characterized by insomnia or excessive sleepiness that is associated with a work schedule that operates during the habitual sleep period.
Impact of Sleep Deprivation: The Real Cost of Missed Zzz’s
-
- Even minor sleep deprivation has significant consequences, which are amplified in high-stakes professions like yours.
- Impaired Decision-Making & Cognitive Function: Reduced ability to think clearly, solve problems, make sound judgments, and recall information. This is critical in emergency situations.
- Reduced Reaction Time: Slower physical and mental responses, increasing the risk of accidents on duty (e.g., driving, operating equipment) and off duty.
- Increased Irritability & Mood Swings: Less patience, higher levels of frustration, and a greater likelihood of emotional outbursts, impacting crew dynamics and personal relationships.
- Weakened Immune System: Chronic sleep deprivation makes you more susceptible to colds, flu, and other infections, leading to more sick days and missed work.
- Higher Risk of Accidents & Errors: Fatigue is a significant factor in human error, which can have severe consequences in your line of work.
Long-Term Health Issues:
Chronic sleep deficiency is linked to increased risk of heart disease, diabetes, obesity, and mental health conditions like depression and anxiety.

Conquering Shift Work Sleep Challenges
You can’t change your job’s demands, but you can adopt strategies to minimize their impact on your sleep. These tips are designed to be practical, whether you’re sleeping at home, the station, or in a temporary lodging.
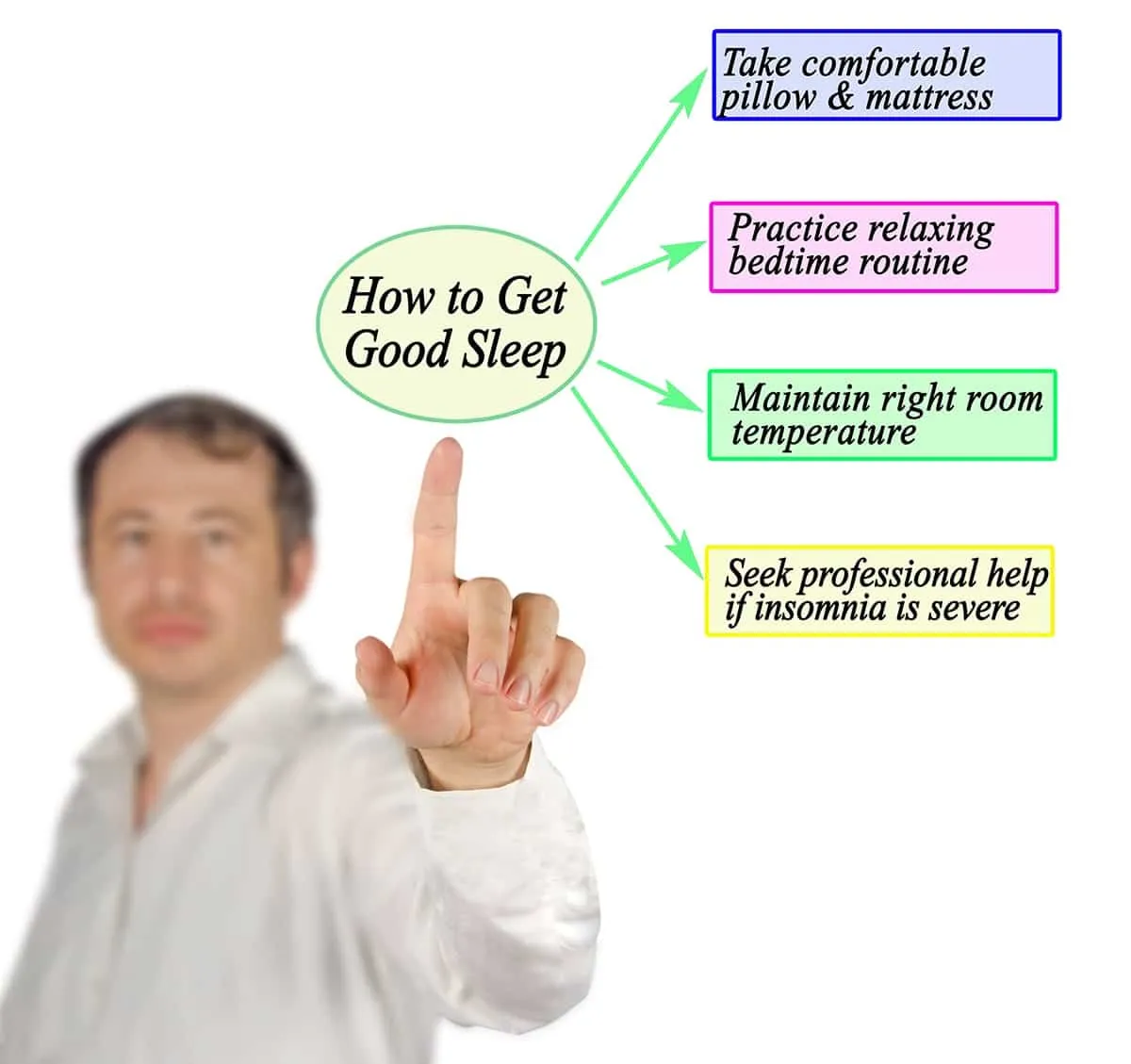
Creating a “Sleep Sanctuary”: Optimize Your Environment
Regardless of when you sleep, make your sleep space as conducive to rest as possible.
-
- Darkness is Key: Even small amounts of light can disrupt melatonin production.
- Blackout Curtains: Invest in high-quality blackout curtains that completely block out daylight.
- Eye Mask: A comfortable sleep mask can be a simple, portable solution.
- Cover All Light Sources: Tape over blinking electronics (smoke detector lights, charging lights) or unplug them.
- Quiet is Crucial: Minimize noise distractions.
- Earplugs: Experiment with different types for comfort and effectiveness.
- White Noise Machine/App: Consistent, soothing sound (e.g., fan, rain, static) can mask sudden noises (traffic, household sounds, station activity).
- Communicate with Family/Housemates: Ask them to be mindful of noise during your sleep times.
- Cool & Comfortable: Your body sleeps best in a cool environment.
- Aim for a room temperature between 18-20°C (65-68°F).
- Ensure comfortable bedding and clothing.
- No Electronics in the Bedroom: Avoid screens (phones, tablets, TVs) for at least an hour before sleep. The blue light emitted by devices suppresses melatonin.
- Darkness is Key: Even small amounts of light can disrupt melatonin production.
Pre-Sleep Routine: Signaling Your Body to Wind Down
Consistency is key, even with varied sleep times. Establish a routine that signals to your body it’s time to prepare for sleep.
-
- Warm Shower or Bath: Helps relax muscles and lowers body temperature slightly afterward, promoting sleep.
- Reading (Physical Book): Calms the mind without screen exposure.
- Gentle Stretching or Yoga: Releases physical tension.
- Mindfulness/Breathing Exercises: (See Module 3) Helps quiet a racing mind.
- Avoid Stimulating Activities: No intense workouts, stressful conversations, or work-related tasks immediately before attempting sleep.
- Aim for Consistency: Try to stick to your wind-down routine every time you prepare for sleep, whether it’s 8 PM or 8 AM.
Post-Shift Decompression: Turning Off Your Mind
This is especially vital after a high-stress call or a demanding shift. Your mind can still be buzzing with adrenaline and replaying events.
-
- “Cool-Down” Period: Don’t go straight from the intensity of a call to trying to sleep. Give yourself a buffer.
- Change Out of Uniform: A symbolic and physical separation from work.
- Listen to Calming Music or a Podcast: Something non-stimulating that helps shift your focus.
- Light Activity: A short, gentle walk (e.g., around the block) can help discharge lingering adrenaline.
- Journaling: Briefly writing down thoughts or concerns from the shift can help clear your mind before bed.
- Avoid “Debriefing” in Your Head: If your mind starts replaying incidents, gently redirect it to your planned relaxation activity.
Managing Caffeine and Alcohol: Be Aware of the Double-Edged Sword
-
- Caffeine: While tempting for energy on shift, caffeine has a long half-life (it stays in your system for hours). Avoid caffeine within 6-8 hours of your intended sleep time. If you’re on a night shift and trying to sleep at 8 AM, your last coffee should be around midnight.
- Alcohol: Alcohol might make you feel drowsy initially, but it significantly disrupts sleep quality later in the night, leading to fragmented sleep and less restorative deep sleep. Avoid alcohol close to bedtime, especially after a tough shift. It can also exacerbate anxiety and depression.
Strategic Napping
Naps can be a powerful tool for combating fatigue, but they need to be used wisely to avoid disrupting your main sleep cycle.
The Power Nap (20-30 minutes):
-
- When: Ideal for boosting alertness and performance during a long shift, or to bridge the gap between a short night’s sleep and an evening event.
- How: Keep it short! A 20-30 minute nap can provide significant refreshment without sending you into deep sleep, which leads to “sleep inertia” (that groggy feeling upon waking).
- Avoid longer naps: Naps longer than 30 minutes can make it harder to fall asleep later for your main sleep period.
Preparation for Night Shifts: Proactive Napping
-
- If you know you have a night shift coming up, a longer “prophylactic” nap (e.g., 60-90 minutes) in the late afternoon before your shift can significantly boost your alertness and endurance for the coming night. This helps to front-load some sleep and make the transition easier.
- Experiment to find what works best for your body without making you feel more tired.
When to Seek Professional Help for Sleep
While good sleep hygiene can make a significant difference, some sleep issues require professional intervention. Don’t hesitate to seek help if your sleep problems are persistent and impactful.
Recognizing Chronic Insomnia, Excessive Daytime Sleepiness, or Other Persistent Sleep Disorders:
-
- You consistently struggle to fall asleep, stay asleep, or wake up feeling unrefreshed, despite applying sleep hygiene techniques.
- You experience excessive sleepiness during the day, even after what you believe was sufficient sleep.
- Your sleep problems are significantly impacting your mood, performance, relationships, or overall quality of life.
- You suspect specific sleep disorders like sleep apnea (loud snoring, gasping, waking up choking), restless legs syndrome, or chronic insomnia.
Information on Sleep Clinics and Specialists in Alberta:
-
- Start with your Family Doctor: They can assess your symptoms, rule out underlying medical conditions, and provide initial guidance.
- Referral to a Sleep Specialist: Your doctor may refer you to a sleep medicine physician or a sleep clinic. These specialists can conduct sleep studies (polysomnography) to diagnose conditions like sleep apnea, narcolepsy, or chronic insomnia.
- Cognitive Behavioural Therapy for Insomnia (CBT-I): This is often considered the most effective long-term treatment for chronic insomnia and is available through many psychologists and therapists in Alberta. It helps you identify and change thoughts and behaviours that prevent you from sleeping well.
- Employee Assistance Programs (EAPs): Your department’s EAP can be a confidential first point of contact for counselling related to sleep issues or for referrals to sleep specialists.
Prioritizing your sleep is a fundamental act of self-preservation and a critical component of your ability to perform your demanding job safely and effectively. Make sleep a non-negotiable part of “1st Health.”